Dr Stephen Dunn, Chief Executive, introduced the day, making a particularly strong point about the importance of getting to know the person, especially with the ageing population increasing, and so too the demands on the NHS. He talked about the importance of recognising delirium and the importance of continual education and further understanding on this subject, both trust-wide and nationwide.
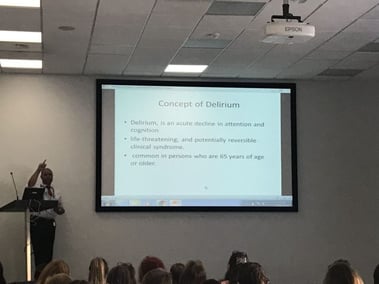
Dr Tito Junco-Russeau, Consultant Geriatrician at WSH described delirium as an acute, life-threatening, and potentially reversible clinical syndrome. He talked about using the right diagnostic tool to determine whether a patient was ‘CAM-POSITIVE’, as the CAM tool (Confusion Assessment Method) was more acceptable than the 4AT tool. He also discussed the risk factors, consequences of delirium, and the importance of non-pharmacological management. He covered all aspects, including possible causes, short and long-term consequences, and included slides for reference.
Jane Gilby, Admiral Nurse, Basildon University Hospital, talked about the role of the admiral nurse, showing the animation of the admiral nurse re-uniting a ‘lost’ dementia patient with her loved one, through music, familiar objects, patience and understanding. She outlined how her role is to support families, carers, hospital and other organisations. Admiral Nurses cover diagnosis, living with dementia, end of life including advance care planning, and spreading information to the ward.
Elizabeth Chapman, Senior Sister, Basildon University Hospital, who talked about how they were one of the first in the Country to set up ‘John’s Campaign, and she showed delegates their resource trolley. She also stressed the importance of visitors, the impact they make, he discussed improvements she has made, i.e. huge yellow signs for the bathrooms, and how important it is to become a ‘dementia friend’ and use many and varied ways to reach patients, i.e. pet therapy, reminiscence rooms, themed surroundings (i.e. a pub-style day room etc)
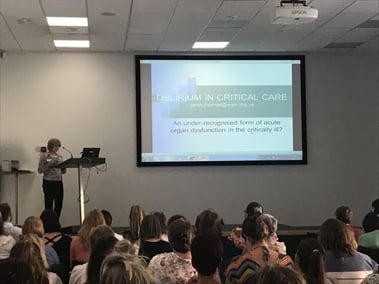
Janet Thomas, Critical Care sister at WSH amazed the delegates by showing how she got her patients mobilized as a matter of priority, as soon as possible, and stressed how non-pharmacological interventions can be used to help prevent or decrease delirium, which can be more prevalent in a Critical Care Unit. An adapted CAM is used for CCU along with the RASS Sedation Assessment, and it is still vital to know what a patient’s baseline is. She also discussed how delirium is a fluctuating, organic mental syndrome which is acute and is reversible. It is not a new phenomenon but is still under-recognised.
Jan Brear, Specialist OT, The Forrest Centre, gave us an insight into ‘Timeslips’ where creative engagement is encouraged through getting patients to create a story, led by Jan, whereby the patient becomes a storyteller. This validates their existence, stimulates, creates self-worth, and is non-patronising and extremely person-centred. It is a reminder that everyone has the capacity to be creative and one is never too old to play, and of course, endorphins are released into the brain during the session. It could be called social role therapy, as even patients with minimal capacity for communication are included, barriers are broken down, there are no wrong answers and meaningful self-expression has been provided, even on the functional mental health wards, not just the organic wards.
Julie Fountain, Lead Nurse Dementia & Frailty and Maggie Woodhouse, Dementia Practitioner and Trainer at WSH talked about delirium being a ‘cognitive superbug’ not to be confused with dementia. They discussed how to differentiate between delirium and dementia, namely that delirium does not start slowly (as dementia does), and the importance of knowing the recent background history of what the patient is normally like. They also discussed about being aware of the quiet, sometimes un-noticed hypo-active delirium patient. Delirium requires more nursing and can result in a complicated discharge, even a new baseline level. They stressed about pain sometimes being a precursor, so also is being moved, and having had previous episodes of delirium, and having sensory impairments. Patients with protracted delirium would certainly need John’s Campaign to maintain normality, and help reduce the number of staff having to treat the person.
Dr Mary McGregor, Consultant in Palliative Care Medicine discussed a case study, and in particular, the issue of having to prescribe for increased pain, which can increase delirium, therefore requiring not only a delicate balancing of how much pain relief to prescribe, without increasing delirium. Sometimes at this end of life stage, relatives will need to be involved, in order to agree to increased tranquilisers being the best option. Approximately 88% of patients close to death will experience delirium. It was also discussed about involving the psychiatric team, as there is a crossover between physical and mental health with delirium.
Pedro Santos, Team Leader, Assistive Technology Team at Northamptonshire Adult Social Services showed delegates the ‘smart’ devices used to help keep patients in their own homes, living independently, with, e.g. family members being alerted when mum walks beyond a designated ‘safe’ area. These devices have to be balanced with what the patient wants, not just what the relative thinks they should have. The devices all feed into a computer, and can be used to assess how mobile a person is, how often they walk to the bathroom each day, and therefore can help predict and potentially avoid water infection, or falls. A ‘virtual house’ can show what devices are available.
There was then a demonstration of the Reminiscence Therapy system as this showed so many different aspects of person-centred care, and how it can ease, calm and distract. The focus of the day was about seeing the person behind their dementia or delirium, and every speaker was passionate about making that happen even more, and spreading the message, through sharing, networking, and going the extra mile.
